This is an E log book to discuss our patients de identified health data shared after guardians informed consent.
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve this patients clinical problems with collective current best evidence based inputs.
This E-book also reflects my patients centered online learning portfolio and your valuable comments in comment box are most welcome.
I have been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency and to comprehend clinical data including history, clinical finding investigations and come up with a diagnosis and treatment plan.
CHIEF COMPLAINTS
- blackish discolouration of the palms and soles since 3 months
- loss of appetite since 3 months
HISTORY OF PRESENTING ILLNESS
The patient was apparently alright 3 months ago then he developed blackish discolouration of the palms and soles which was insidious in onset, not associated with pain, itching, difficulty in movements. He works in agriculture mainly for watering the crops (works only one shift from 5 am to 1 pm) the rest of the day he spends at home watching television. He used to work in a company which produces insulators for the electrical wires from 2006 to 2012 and was worried if that may have caused his condition. For a few months he also worked as a security guard.
Fatigue was present since 3 months
He also complained of decreased appetite since 3 months to all kinds of food
Last week he also developed an injury to the lateral side of the right leg which is healing rather slowly and also developed a spontaneous ulcer on the mid leg 3 days ago.
Since 4-5 days he has developed aversion to food and doesn't even want to place food in his mouth.
PAST HISTORY
H/O similar complaints in the past in 2016 when he developed blackish discolouration and he went to a hospital in hyderabad for treatment where he claims they gave unknown injections once per week for 3 weeks after which his symptoms alleviated and then he claims to be asymptomatic since the episode in 2016 till 3 months ago.
No H/O Hypertension, DM, asthma, epilepsy, CAD, CVA, thyroid disorders
H/O vasectomy 27 years ago
FAMILY HISTORY
No similar complaints in the family
PERSONAL HISTORY
DIET: Mixed
APPETITE: decreased
SLEEP: adequate
B&B: Regular
He consumes alcohol socially
No allergies
GENERAL EXAMINATION
The patient was conscious, coherent, cooperative, well oriented to time, place, person. He was moderately built and moderately nourished.
Pedal edema present on the right ankle which is pitting type
Tenderness present in the circled area
Pallor present
No icterus, cyanosis, clubbing, lymphadenopathy
VITALS:
Temperature: Afebrile
BP: 110/70 mm Hg
PR: 84 bpm
RR: 18 cpm
SYSTEMIC EXAMINATION
RESPIRATORY SYSTEM:
UPPER RESPIRATORY TRACT:
No halitosis, post nasal drip, tonsils, dental caries, dns, polyps, sinus tenderness
Oral hygiene present
LOWER RESPIRATORY TRACT:
INSPECTION:
Chest is symmetrical in shape
Trachea is in the midline (trails sign)
Apical impulse not visualised
No drooping of shoulder, supraclavicular and infraclavicular hollowing, indrawings, retractions, crowding of ribs
No pectus carinatum, pectus excavatum, kyphoscoliosis, winging of scapula
No sinuses, scars, dilated veins, nodules
Normal movements with respiration
PALPATION:
No local rise of temperature
All inspectory findings confirmed
Expansion of the chest is symmetrical
Tactile vocal fremitus: normal
PERCUSSION:
Resonant note
AUSCULTATION:
Normal
CVS:
S1, S2 heard
PER ABDOMEN:
Soft non tender
CNS:
No focal neurological deficits
PROVISIONAL DIAGNOSIS:
Anaemia secondary to ?B12 deficiency
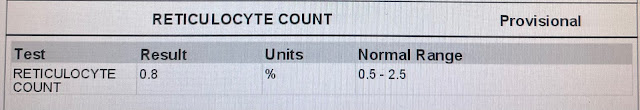
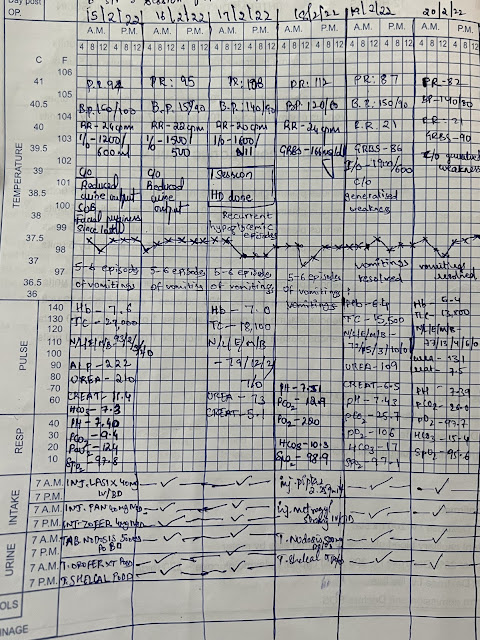
INVESTIGATIONS:
01/08/2023
























Comments
Post a Comment