THE CASE OF A 45 YEAR OLD FEMALE WITH OLIGURIA AND SOB
This is an E log book to discuss our patients deidentified health data shared after guardians informed consent.
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve this patients clinical problems with collective current best evidence based inputs.
This E-book also reflects my patients centered online learning portfolio and your valuable comments in comment box are most welcome.
I have been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency and to comprehend clinical data including history, clinical finding investigations and come up with a diagnosis and treatment plan.
CHIEF COMPLAINTS
- Reduced urine output since 1 week
- Easy fatiguability since 1 week
- Shortness of Breath since three days
HISTORY OF PRESENTING ILLNESS
The patient was apparently asymptomatic 2 years back then the patient developed a fever followed by many bouts of vomiting and puffy face. The patient also had right loin pain, reduced urine output and generalised anasarca. The patient got worried and went to a hospital in Nalgonda where they live. A diagnosis was made and the patient was sent to Gandhi hospital where she underwent DJ stenting and dialysis. The patient underwent dialysis for about 5-6 times and then due to the pandemic she went back to her normal life. Since then she went on with her work until 6 months ago when she stopped going to work as she was fatigued all the time. She is a labourer by occupation. She also developed grade 4 shortness of breath and had a puffy face at the time of admission. The patient also had 5-6 episodes of vomiting over the few days.
PAST HISTORY
- H/O hemodialysis for 5-6 sessions 2 years back
- No H/O Diabetes, hypertension, epilepsy, tuberculosis, asthma
PERSONAL HISTORY
- Diet: mixed
- Appetite: normal
- Sleep: adequate
- Bowel and bladder: normal
- Allergies: absent
- No addictions
GENERAL EXAMINATION
Patient was conscious, coherent, cooperative and well oriented to time, place and person. The patient was moderately built and nourished. Pallor is present but no icterus, clubbing, lymphadenopathy present.
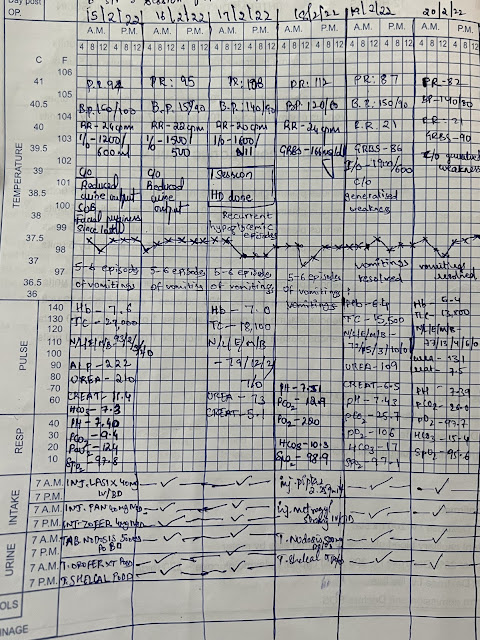
VITALS AT ADMISSION:
BP: 160/100
RR: 22 CPM
PR 74 BPM
TEMPERATURE: AFEBRILE
 |
SYSTEMIC EXAMINATION:
- CVS: S1, S2 heard, no murmurs or added sounds present
- RS: BAE +
- ABDOMEN: Soft and tender
- CNS: no focal neurological deficits
PROVISIONALS DIAGNOSIS:
Chronic Kidney Disease on MHD
TREATMENT PLAN:









Comments
Post a Comment