This is an E log book to discuss our patients de identified health data shared after guardians informed consent.
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve this patients clinical problems with collective current best evidence based inputs.
This E-book also reflects my patients centered online learning portfolio and your valuable comments in comment box are most welcome.
I have been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency and to comprehend clinical data including history, clinical finding investigations and come up with a diagnosis and treatment plan.
CHIEF COMPLAINTS
Chest pain since 1 month
HISTORY OF PRESENTING ILLNESS
The patient was apparently alright 1 month ago then he developed chest pain around the same time he developed Dengue Fever with Thrombocytopenia. The pain was sudden in onset and localised at the left 5th intercostal space, sharp pain, non radiating, aggravated on coughing and work (bending and lying down) and was reduced by itself after 5 minutes. It is associated with shortness of breath.
H/O cough with expectoration (white)
Not associated with palpitations, tremors and sweating.
Fatigue was present
No H/O dizziness, headache, burning micturition
No H/O loose stools
He also developed bilateral knee pains since 6 months
PAST HISTORY
H/O Hypertension since two years
No H/O DM, asthma, epilepsy, CAD
H/O dengue fever with thrombocytopenia one month ago
H/O surgery for hydrocele 20 years ago
FAMILY HISTORY
No similar complaints in the family
PERSONAL HISTORY
DIET: Mixed
APPETITE: decreased
SLEEP: inadequate
B&B: Regular
Addictions: known alcoholic since 40 years but stopped 2 months ago.
No allergies
GENERAL EXAMINATION
The patient was conscious, coherent, cooperative, well oriented to time, place, person. He was moderately built and moderately nourished.
No pallor, icterus, cyanosis, clubbing, lymphadenopathy
VITALS:
Temperature: Afebrile
BP: 110/60 mm Hg
PR: 84 bpm
RR: 18 cpm
SYSTEMIC EXAMINATION
UPPER RESPIRATORY TRACT:
No halitosis, post nasal drip, tonsils, dental caries, dns, polyps, sinus tenderness
Oral hygiene present
LOWER RESPIRATORY TRACT:
INSPECTION:
Chest is symmetrical in shape
Trachea is in the midline (trails sign)
Apical impulse not visualised
No drooping of shoulder, supraclavicular and infraclavicular hollowing, indrawings, retractions, crowding of ribs
No pectus carinatum, pectus excavatum, kyphoscoliosis, winging of scapula
No sinuses, scars, dilated veins, nodules
Normal movements with respiration
PALPATION:
No local rise of temperature
All inspectory findings confirmed
Expansion of the chest is symmetrical
Tactile vocal fremitus: normal
PERCUSSION:
Resonant note
AUSCULTATION:
Normal everywhere except the left inframammary area where crepts can be heard.
CVS:
S1, S2 heard
PER ABDOMEN:
Soft non tender
CNS:
No focal neurological deficits
PROVISIONAL DIAGNOSIS:
Pleuritic chest pain
INVESTIGATIONS:
06/12/2022
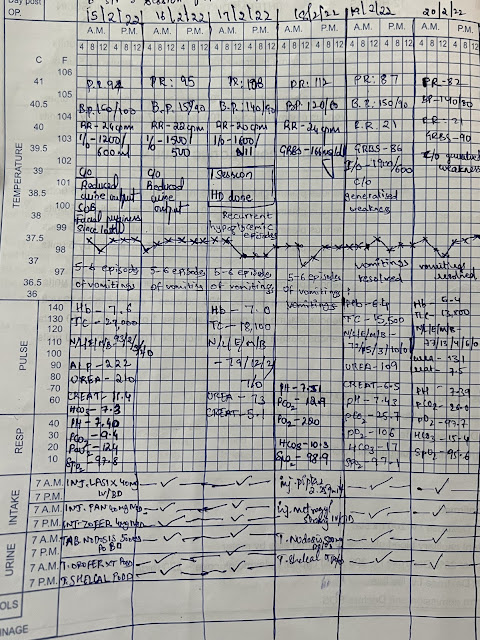
TREATMENT:
1. T. ULTRACET
2. T.SHELCAL









Comments
Post a Comment