A 65 YEAR OLD MALE WITH WEAKNESS IN ALL LIMBS
This is an E log book to discuss our patients de identified health data shared after guardians informed consent.
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve this patients clinical problems with collective current best evidence based inputs.
This E-book also reflects my patients centered online learning portfolio and your valuable comments in comment box are most welcome.
I have been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency and to comprehend clinical data including history, clinical finding investigations and come up with a diagnosis and treatment plan.
CHIEF COMPLAINTS
⬩ Altered gait since 2 year
⬩ Unable to walk since 3 months
⬩ Stiffness of all limbs since 15 days
⬩ decreased appetite since 15 days
⬩ weakness of all limbs since 15 days
⬩ unresponsiveness since 4 days
HISTORY OF PRESENTING ILLNESS
The patient was alright 2 years ago then he started developing generalised weakness, and complained that he felt like he was walking on pins few times. Generalised weakness caused him to stop working as a goldsmith which he has been doing since his youth. He would still do his own activities like bathing, eating, brushing etc. His routine before included him waking up at 5 am and carrying out his daily activities like brushing, bathing and eating his breakfast before going to work. He would work until 4 pm and then resume his other activities till sleep.
Now he would spend the majority of his time watching tv and carrying out his other routine activities except going to work.
1 year ago he started feeling intermittent weakness in his limbs and feeling pins and needles sensation on his feet. The weakness was gradual in onset and progressing and intermittent. He would go out even less now and spent majority of his time on the bed, uninterested to even watch tv. He was being taken to the hospital multiple times but with no proper diagnosis.
6 months ago he started being scared of walking as he was scared he would fall down, and the pricking sensation in the foot increased.
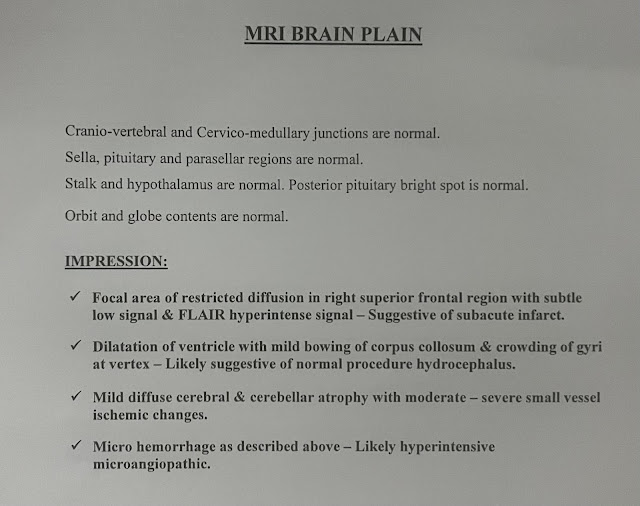
3 months ago he was taken to a hospital on one such episode of weakness, where they took a MRI in Nalgonda which showed:
- Hydrocephalus
- early Parkinson's changes
They advised to relieve the CSF pressure but due to financial reasons they did not go forward with the procedure.
20 days ago he developed typhoid fever which was diagnosed locally after which he deteriorated even more.
15 days ago he developed stiffness of all the limbs and also weakness in all the limbs. His wife massaged his legs with oil with which his symptoms relieved a little.
15 days ago he started eating less ( decreased appetite )
5 days ago he stopped feeding completely.
3 days ago he developed fever not associated with chills and rigours and became unconscious.
PAST HISTORY
Known case of hypertension since 5 years
Known case of diabetes since 3 years - taking glimipiride 2 mg + metformin 500 mg
No H/O epilepsy, asthma, tuberculosis, CAD
TREATMENT HISTORY
- antihypertensives ( drug unknown )
- oral hypoglycemics - glimipiride 2 mg + metformin 500 mg
- NSAIDS frequently
PERSONAL HISTORY
Diet: mixed
Appetite: decreased
Sleep: adequate
Bowel and bladder: normal
No allergies
Chronic alcoholic since he was 20 years of age and stopped 2 years back - he used to take 250 ml everyday
FAMILY HISTORY
No known family history
GENERAL EXAMINATION
The patient is conscious, not coherent, not cooperative, not oriented to time, place and person.
He is poorly built and malnourished.
VITALS
Temperature: afebrile
BP: 110/70 mm Hg
HR: 92 bpm
RR: 22 cpm
SpO2: 96 %
Pallor present
Skin pinch test:
No cyanosis, icterus, clubbing, lymphadenopathy, edema
SYSTEMIC EXAMINATION
CVS: S1, S2 heard, no murmurs
RESP: NVBS, BAE
PER ABDOMEN: soft, non tender
CENTRAL NERVOUS SYSTEM:
Higher mental function: conscious, non coherent, not oriented to time, place and person.
Language - APHASIC
Unable to write or read
GCS ( Glassgow coma scale)
Eye opening: to speech - 3
Verbal response: no response - 1
Motor response: flex to withdraw from pain - 4
Total score: 8
SENSORY SYSTEM: Cannot be examined
MOTOR SYSTEM: Muscle wasting present, no cramping, no involuntary movements.
CRANIAL NERVE EXAMINATION:
CN 1: OLFACTORY NERVE
CN 2: OPTIC NERVE
CN 3: OCULOMOTOR NERVE - Normal
CN 4: TROCHLEAR NERVE - Normal
CN 5: TRIGEMINAL NERVE - Normal
CN 6: ABDUCENS NERVE - Normal
CN 7: FACIAL NERVE - Normal
CN 8: VESTIBULOCOCHLEAR NERVE
CN 9: GLOSSOPHARYNGEAL NERVE - gag reflex present
CN 10: VAGUS NERVE - difficulty in sleep
CN 11: SPINAL ACCESSORY NERVE
CN 12: HYPOGLOSSAL NERVE
TONE: Hypertonicity in flexors and extensors of both upper and lower limbs
All the limbs were in flexed positing.
Lead pipe rigidity seen.
POWER:
3/5 in the upper limbs
Lower limbs power couldnt be elicited
REFLEXES:
SUPERFICIAL:
- Corneal reflex: present
- Conjunctival reflex: present
- Abdominal reflex: present
- Plantar reflex: present
DEEP:
UPPER LIMB:
No meningeal signs
Gait cannot be seen
PROVISIONAL DIAGNOSIS
- Altered sensorium due to hypovolemic hyponatremia
- Parkinson’s disease
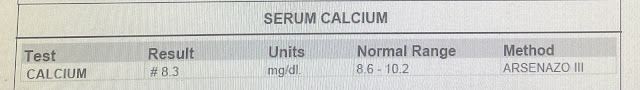
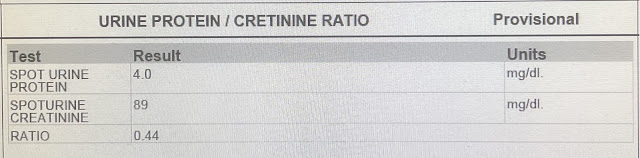
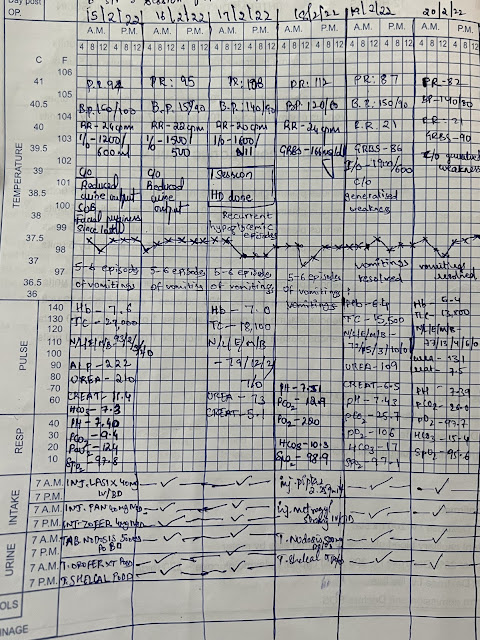
INVESTIGATIONS
TREATMENT
- 3% NACL @ 15 ml/ hr- Head end elevation upto 30 degrees- Ryles tube feeding- Ringer lactate - Normal Saline - Syndopa
- 3% NACL @ 15 ml/ hr
- Head end elevation upto 30 degrees
- Ryles tube feeding
- Ringer lactate
- Normal Saline
- Syndopa





















Comments
Post a Comment