This is an E log book to discuss our patients de identified health data shared after guardians informed consent.
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve this patients clinical problems with collective current best evidence based inputs.
This E-book also reflects my patients centered online learning portfolio and your valuable comments in comment box are most welcome.
I have been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency and to comprehend clinical data including history, clinical finding investigations and come up with a diagnosis and treatment plan.
CHIEF COMPLAINTS
- Fever since 6 months
- Reduced appetite since 6 months
- Cough since 3 months
- Shortness of breath since 3 months
HISTORY OF PRESENTING ILLNESS
The Patient was apparently alright 6 months ago, then he developed itching which was all over the body and for which he went to a local hospital where they suggested that he start dialysis, and he had 2 sessions where they introduced a cannula into the vein of his neck. After which he developed extreme pain, fever and headache, thus they stopped. The fever was intermittent and only reducing on taking drugs and then reappearing. 15 days ago they brought him to the opd and was admitted and the fever has been continuous since reducing on medication. He also developed decreased appetite and gives a history of loss of weight.
PAST HISTORY
In 2015 the patient was diagnosed with hypertension
In 2016: the patient was diagnosed with dengue and was investigated and treated symptomatically where it was revealed that his creatinine and uric acid levels were high and was then given medications to decrease the levels.
During this time the patient also complains of joint pains and swelling when eating certain foods which were sour like tamarind, and also red meats (accumulation of uric acid)
He would also feel nauseous at times but rarely vomited.
6 months ago the patient developed severe pruritis after which he was taken to the hospital where they suggested he start dialysis and 2 such sessions were done after which he developed the fever. At this point before dialysis his creatinine levels were 6.2, blood urea- 145.
6 months ago he was diagnosed with CKD.
No H/O diabetes, epilepsy, tuberculosis, CAD, asthma
FAMILY HISTORY
His mother is a known case of hypertension
PERSONAL HISTORY
DIET: Mixed
APPETITE: decreased
SLEEP: inadequate
B&B: irregular
Chronic alcoholic since 30 years, 90 ml per day, stopped 6 months ago after the onset of rash.
Allergic to peanuts
TREATMENT HISTORY
T.metXL 25 mg
GENERAL EXAMINATION
The patient was conscious, coherent, cooperative, well oriented to time, place, person. He was moderately built and moderately nourished.
Pallor: Present
No icterus, cyanosis, clubbing, lymphadenopathy
Pedal edema: present, pitting type
VITALS:
Temperature: Afebrile
BP: 140/90 mm Hg
PR: 82 bpm
RR: 16 cpm
SYSTEMIC EXAMINATION
RESPIRATORY SYSTEM:
Inspection:
Oral cavity, nose, pharynx normal
Position of trachea central
Position of apex beat normal
Bilaterally symmetrical
No chest deformities
No spinal deformities
Movements of the chest:
- normal rate
- normal rhythm
Palpation:
Position of trachea: central
Symmetrical chest expansion
No tenderness
Vocal fremitus
Percussion:
Dull note heard all over the chest
Auscultation:
CVS - S1, S2 heard
P/A: soft, non tender
CNS: NAD
PROVISIONAL DIAGNOSIS:
CKD on MHD
INVESTIGATIONS:
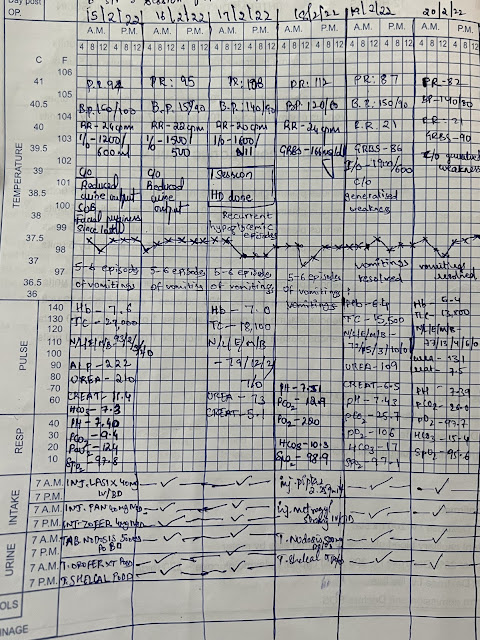
DEC 1
DEC 3
DEC 4
DEC 5
DEC 7
DEC 8
DEC 10
DEC 13
DEC 14
DEC 15
DEC 16
TREATMENT:

















































Comments
Post a Comment