This is an E log book to discuss our patients de identified health data shared after guardians informed consent.
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve this patients clinical problems with collective current best evidence based inputs.
This E-book also reflects my patients centered online learning portfolio and your valuable comments in comment box are most welcome.
I have been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency and to comprehend clinical data including history, clinical finding investigations and come up with a diagnosis and treatment plan.
CHIEF COMPLAINTS
- Fever since 4 days
- Cough since 4 days
- Pedal oedema since 4 days
- Dyspnoea since 3 days
HISTORY OF PRESENTING ILLNESS
The Patient was apparently asymptomatic 4 days ago. Then one day she developed cold and fever which was continuous but relieved on medication, followed by cough with associated with purulent sputum. Then she developed bilateral joint pains (ankle, knee, hip, proximal arm) and pitting edema which was insidious in onset, gradually progressing with no aggravating or relieving factors. She also had dyspnoea at rest (NYHA-4) which was gradually progressing. She also complained of pins and needles sensation in the palms and thighs.
PAST HISTORY
No H/O DM, HTN, asthma, epilepsy, CAD
She had proximal muscle weakness which manifested as difficulty in getting up from squatting position, lifting neck. She also had distal muscle weakness which manifested as difficulty in buttoning and bringing food to the mouth, combing hair etc from 1 year.
Difficulty walking from 1 year
C/O loss of taste since 8 months
C/O throat pain since 8 months
The patient had similar complaints 2 months ago, she went to a health care facility with complaints of knee pain, itching over the neck, proximal and distal muscle weakness and dyspnoea. Also had malar rash which was initially erythematous but later became hyperpigmented. She also had vaginal discharge.
The patient was diagnosed with DERMATOMYOSITIS and was on corticosteroids ( Prednisolone)
The pictures from that are:
Gottrons papules:
They performed a ANTI NUCLEAR ANTIBODY immunofluorescence which showed
Homogeneous pattern. Intensity 4+ the assosiated antigens involved are: dsDNA, Histones.
Clinical association - SLE, Drug induced lupus
They also performed an HRCT which showed: few patchy areas of ground glass opacities in peri bronchovascular distribution- s/o pneumonitis
The TREATMENT protocol was:
1.TAB.CALTEN
2.TAB.AUGMENTIN
3.TAB.NAPROXEN SODIUM
4.TAB.FOLVITE
5.CANDID CREAM
6.TAB.WYSOLONE
7.TAB.ESOMEPRAZOLE
8.TAB.SODIUM ALENDRONATE WEEKLY ONCE.
MENSTRUAL HISTORY
Menarche: 11 years
Cycle lasts: 26-28 days
3 days of menstruation
Regular cycles
No pains or clots
MARITAL HISTORY
She is married but doesn't have any kids, she has adopted a girl from her sister in law.
She has primary infertility.
FAMILY HISTORY
No similar complaints in the family
PERSONAL HISTORY
DIET: Mixed
APPETITE: decreased
SLEEP: inadequate
B&B: irregular
No addictions
No allergies
GENERAL EXAMINATION
The patient was conscious, coherent, cooperative, well oriented to time, place, person. She was moderately built and moderately nourished.
Pallor: Present
No icterus, cyanosis, clubbing, lymphadenopathy
Pedal edema: present
Facial edema present
VITALS:
Temperature: Afebrile
BP: 150/100 mm Hg
PR: 114 bpm
RR: 30 cpm
SYSTEMIC EXAMINATION
CVS - S1, S2 heard
RS: BAE +
P/A: soft, non tender
CNS: NAD
PROVISIONAL DIAGNOSIS:
DERMATOMYOSITIS
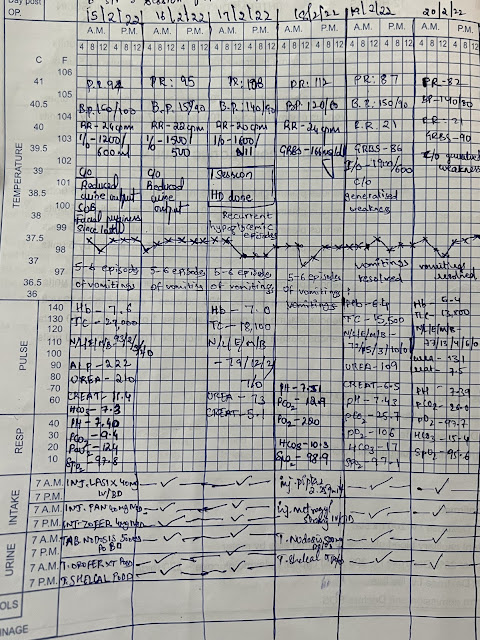
INVESTIGATIONS:
TREATMENT:
1.T.SEPTRAN DS TID
2.TAB.FLUCONAZOLE 150 MG OD
3.OINT.CANDID MOUTH PAINT IN ORAL CAVITY
4.TAB.WYSOLONT 50 MG OD
5.TAB.FOLIC ACID 5 MG ONCE A WEEK.













Comments
Post a Comment